Technology has a significant impact on how operations are run more efficiently and how well patients do. Software integrations are unique among technical innovations in that they improve the interoperability and functionality of healthcare systems.
From hospitals to private offices, these interfaces guarantee smooth communication and data interchange across a range of healthcare platforms.
This article explores the major software integrations used in the US healthcare industry, emphasizing how they maintain compliance with health standards, enhance patient care, and expedite workflows.
Understanding Electronic Health Records (EHR)
An essential component of contemporary healthcare are electronic health records, or EHRs, which are computerized copies of patient paper documents. EHRs are patient-centered, real-time records that give authorized users quick, secure access to information.
An extensive picture of a patient’s medical history, diagnosis, prescriptions, treatment plans, dates of immunizations, allergies, radiological images, and laboratory and test results can be found in electronic health records (EHRs), in contrast to traditional paper records.
Through a variety of interfaces, this system provides direct or indirect support for other care-related tasks, such as quality monitoring, outcomes reporting, and evidence-based decision support. EHRs are intended to collect, organize, and preserve patient data as well as facilitate communication between various healthcare providers, improving the continuity of care.
Redefine Your Business with Digital Transformation
Innovative Digital Solutions, Designed for Your Unique Needs
Explore Digital TransformationTelehealth Integration
The field of telehealth has changed the face of healthcare, as seen by the COVID-19 pandemic, which made remote clinical treatments necessary due to physical distance. Technologies that provide virtual medical, health, and educational services are referred to as telehealth.
It is now crucial to incorporate telehealth features into practice management and electronic health record (EHR) systems. With the help of this connection, healthcare professionals may now give patients with remote real-time care through virtual consultations.
By continuously monitoring patient health data and transmitting information to healthcare practitioners via digital technology, it also facilitates remote patient monitoring. Integrating secure communication channels into EHR systems guarantees that all patient interactions and data are kept private, available only to authorized people, and compliant with privacy laws.
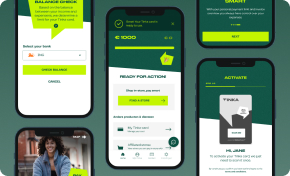
Mobile App Development for a Competitive Edge
Developing Mobile Apps that Engage Your Customers with Your Brand
Explore Mobile App DevelopmentePrescribing Integration
Prescription management and fulfillment are being completely transformed by electronic prescribing, or ePrescribing. Bypassing the conventional paper-based procedure, it enables healthcare providers to electronically deliver prescriptions to pharmacies.
Simplifying the drug management procedure, ePrescribing with EHR systems improves the functionality of healthcare delivery. By sending precise and readable prescription data straight to the pharmacist, this integration lowers the risk of prescription errors—such as those brought on by handwritten or manual entry. It also aids in monitoring prescription fulfillment and patient adherence to treatment plans.
Cross-referencing the patient’s electronic health record with the prescription, ePrescribing systems can notify physicians about possible drug interactions, erroneous dosages, and patient allergies.
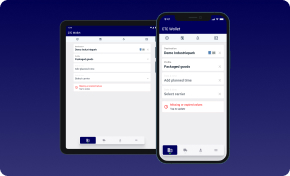
Experience the Power of Custom Software Development
Transformative Software Solutions for Your Business Needs
Explore Custom SoftwareClinical Decision Support (CDS) Integration
Systems known as clinical decision support (CDS) give medical professionals patient-specific evaluations or suggestions to help with clinical decision-making.
Using extensive Electronic Health Records (EHR) data, these systems can provide prompt, patient-specific information that improves safety and quality of care. At the point of care, clinicians can access up-to-date, clinically best practices and evidence-based guidelines by integrating CDS technologies with EHR systems.
Through warnings, reminders, and clinical recommendations, this integration can greatly improve the efficacy of clinical care by aiding the early detection and management of illness conditions. In order to reduce treatment plan variability and guarantee that all patients receive the best care possible based on the most recent medical research and regulatory compliance standards, CDS helps standardize care delivery across a variety of healthcare settings.
Leading Research & Development for Your Success
Driving Innovation in Every Product Aspect Through R&D-Driven Software
Learn About R&D ServicesMedical Billing Integration
The billing and claims process is made simpler by integrating medical billing software with EHR and practice management systems. Streamlining payment collection and insurance claim administration need this connectivity. The administrative load on billing personnel and healthcare providers is lessened when insurance eligibility verification, claim filing, and payment processing are done automatically.
Medical billing software and patient data are directly linked, guaranteeing that billing procedures are founded on current and accurate patient interactions and treatments.
This lowers billing errors, quickens the reimbursement cycle, and raises the possibility that insurance claims will be approved on time and accurately.
Integrated medical billing systems can offer analytics and reporting capabilities that support healthcare organizations in tracking their financial performance, seeing patterns in payment delays or denials, and modifying their billing procedures to strengthen their financial position.
Reducing billing-related errors and delays in care delivery, this integration maximizes revenue streams and improves patient satisfaction.
Laboratory Information Systems (LIS) Integration
Medical laboratory operations such as handling specimens, storing data, and tracking lab orders and findings depend heavily on Laboratory Information Systems (LIS).
The diagnosis procedure can be streamlined by electronically ordering lab tests straight from the patient’s record when LIS is integrated with Electronic Health Record (EHR) systems.
The danger of errors associated with manual entry is decreased by this seamless integration, which guarantees that test orders are accurate and represent the patient’s actual health status.
The EHR is immediately updated with test results as soon as they are available, giving medical professionals instant access to vital diagnostic data. Faster and more accurate diagnosis and treatment are made possible by this timely access to test findings, which enhances patient outcomes.
Furthermore, by reducing redundant testing and related expenses, LIS integration improves operational effectiveness, which is advantageous to patients and healthcare providers.
Radiology Information Systems (RIS) and PACS Integration
Medical imaging and related data are managed by specialized healthcare information systems called Radiology Information Systems (RIS) and Picture Archiving and Communication Systems (PACS). PACS is devoted to storing, retrieving, presenting, and sharing medical pictures, whereas RIS oversees the scheduling, resource management, and reporting of radiology services.
The administration and accessibility of radiology reports and medical pictures are improved by integrating RIS and PACS with EHR systems. Along with other patient medical records, this integration offers a centralized platform with images and data from multiple imaging modalities, including MRIs, CT scans, and X-rays.
Healthcare professionals have a thorough understanding of a patient’s medical history because to the availability of detailed imaging data in EHRs, which improves the accuracy and knowledge of clinical judgments.
Additionally, this integration speeds up access to imaging tests, promoting better collaboration between medical specialists and improves the precision of diagnosis and treatment planning.
As a result, patient care significantly improves in terms of coordination and quality, and healthcare delivery becomes more efficient.
Health Information Exchange (HIE) Integration
The safe and dependable electronic exchange of health-related data between healthcare institutions is known as health information exchange, or HIE.
The seamless sharing of patient data between various healthcare systems and providers is made possible by the integration of HIE systems with Electronic Health Records (EHR), which improves care coordination and continuity.
Facilitating real-time access and sharing of vital patient data, including lab results, medical histories, and prescription information, this connection helps healthcare providers prevent medical errors and unnecessary testing.
IT Consultancy Designed Around Your Business Objectives
Expert Guidance to Optimize Your Technology Strategy
Discover IT ConsultingBecause it guarantees that every member of the care team has access to the same data, it also facilitates more informed decision-making and effective management of chronic diseases.
Using safe, standardized data sharing techniques, HIE integration supports adherence to patient privacy laws. Integration of HIE leads to a more comprehensive view of a patient’s medical history, which enhances both the overall effectiveness of healthcare delivery systems and patient outcomes.
Standards and Compliance
Healthcare system and application integration is highly dependent on a number of standards that guarantee safe, effective, and uniform data sharing.
Digital Imaging and Communications in Medicine (DICOM), Fast Healthcare Interoperability Resources (FHIR), and Health Level Seven International (HL7) are a few of these. In order to assist clinical practice and the administration, provision, and assessment of healthcare services, HL7 standards enable the interchange, integration, sharing, and retrieval of electronic health information.
FHIR is a more recent standard that supports RESTful designs and makes implementation easier without compromising information integrity. This makes it ideal for cloud communications, mobile applications, and EHR-based data sharing.
In order to guarantee interoperability across imaging systems and modalities, DICOM standardizes the exchange and administration of medical imaging information and related data.
Adherence to these standards is crucial in order to facilitate functional integration and guarantee that data exchanges adhere to strict security and privacy protocols.
Healthcare businesses can nurture a more connected and effective healthcare system by adhering to these standards, which can improve operational efficiencies, ensure regulatory compliance, and improve patient safety.
Enhancing Healthcare Through Strategic EHR Integrations
Patient care efficiency, safety, and quality are greatly improved in the US healthcare industry by integrating critical software systems.
These interfaces assist healthcare professionals in providing more coordinated and individualized treatment by smoothly integrating EHRs, telehealth platforms, ePrescribing tools, clinical decision support systems, medical billing software, and other essential healthcare technology.
It is impossible to overestimate the contribution that HL7, FHIR, and DICOM standards make to the safe and effective interchange of data between healthcare organizations and platforms. They guarantee that these systems function in concert with one another.
Get in touch with HyperSense right now if you’re prepared to learn more about how EHR connections can help your healthcare company. In order to achieve better patient outcomes and operational excellence, let us assist you in navigating the complexity of healthcare technology.